Choosing Death
By Myron Gananian (October 2023)
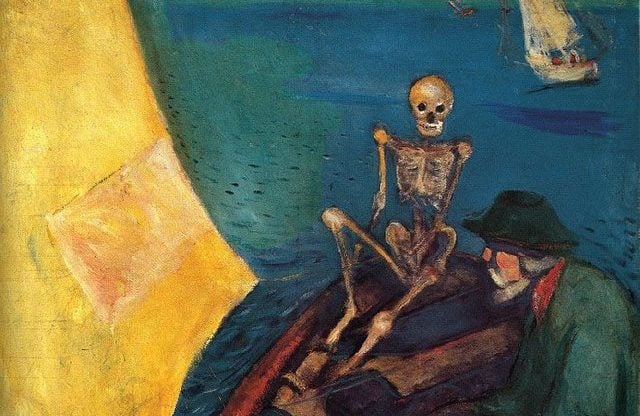
Death at the Helm, Edvard Munch, 1893
“You sure as hell can!”
I heard those words one time in a special context and have never forgotten them, since the occasions for which they were spoken have not ceased to recur. They have retained their special meaning, having been uttered by a highly esteemed surgeon, colleague, and friend. He rather spat them out, without rancor and a tone that brooked little doubt, as if those few words covered volumes of thoughtful concern.
What occasioned his feelings was the too-oft plea of concerned family members when their relative either refuses or is unable to eat: “Doctor, you can’t let him starve to death!” In recognition of current societal concerns focusing on these issues starving to death has many—if not admirable then at least attractive—aspects.
Before addressing the physiological consequences of starvation, it would do well to touch on contentious end of life issues that are currently poorly managed, such as Death Panels and Assisted Suicide, and now, as in Canada, Euthanasia, which would be cast in the shadows by a more humane and widely accepted mode which could ease the path to death. Further, the enormous cost of in-patient care for the terminal patient could be significantly diminished. Under the unassailable effects of benevolence and humanity we are seeing not life prolonged, but death. The memory of families of their beloved dead is so often those final, prolonged days of pain poorly addressed by drugs compounded by urinary and intestinal problems, along with vomiting and bedsores. A loss of dignity in contrast with a full life. The emotional cost exceeds the financial one, the latter often unconscionable. Unfortunately, hospice care is sometimes unnecessarily protracted.
It is an error to regard such considerations from the viewpoint and desires of the non-patient. The dying patient’s situation and needs supersede everyone else’s. To force feed, place tubes through the nose and abdominal wall into the stomach without the clear consent of the patient is patently battery. The attitude that most often leads to violating the patient’s best interest is the family’s inability to finally let go of the beloved and thereby prolong the good-by at the expense of the dying. Treatment at this time cannot be dictated by the family’s wishes if in conflict with the most compassionate care that can be mustered compatible with the patient’s wishes.
Which brings us to starvation. Not only have the consequences of starvation been investigated repeatedly in prisoners declaring hunger strikes, but in terminal patients as well. There are many volunteer organizations that support VSED, Voluntarily Stop Eating and Drinking, a recognized method implementing the cessation of intake of food and drink as an acceptable end of life measure, one advantage of which is the avoidance of any legal or religious taint on the process. Another is the ease of adaptability to hospice care. The right of the patient to refuse nutrition has been certified by the Supreme Court in the Nancy Cruzan case.
What makes VSED particularly suitable for the dying patient is the paucity of serious side effects, most of which can be managed by procedures well established in hospice. If a patient is undernourished the process may take no longer than a couple of weeks. The period of hunger often ends after several days, and as the metabolism of carbohydrates ends with its depletion the burning of fat stores starts and results in ketosis, a situation that provides more energy for the brain than glucose, often resulting in a state not unlike euphoria but, in addition, agitation. After the fat stores are depleted, protein is metabolized resulting in organ failure.
Our society cannot continue to disregard the folly and cruelty of futile efforts in health care. Terminal patients in ICU or anywhere in the hospital are an affront not only to the patient but to our health care system. Hospice care has been a Godsend, and it is possible to make it even more valuable if patients and families would adopt the tenets of VSED.
No techniques touching on end-of-life issues are of value if allowed to be formulated at the worst possible time, near or at the end. No method can best the preparation that anticipation can provide. These issues must be discussed and values expressed as forthrightly as family dynamics allow. The bedside is the worst possible time and place to address these issues and to satisfy all parties involved. Having a long absent, guilt-ridden family member fly in from a distance and attempt to have a role in complicated decisions is a guarantee for mayhem. As diplomatically as possible those who anticipate aiding the terminally ill should encourage as much detailed expression of the patient’s wishes with foresight for this once-in-a-lifetime event.
Even well-worded Medical Directives, POLST documents, and Vial of Life alerts on the refrigerator door are no guarantee that the patient’s wishes will be respected. Nothing supersedes the verbal expression of the patient. His words are final.
Table of Contents
Myron Gananian is a retired physician living in California.
Follow NER on Twitter @NERIconoclast