Covid and the Concierge
A Patient’s Perspective
by G. Murphy Donovan (August 2020)
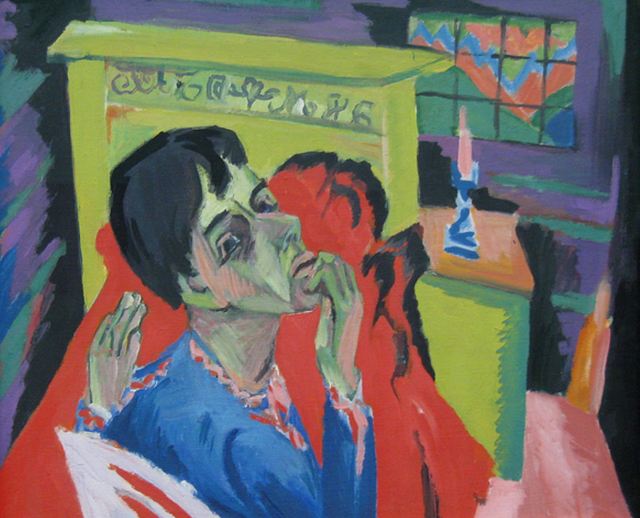
Sick Man, Ernst Ludwig Kirchner, 1918
No crisis unfolds without opportunities. The Covid-19 epidemic is no exception.
Surely the American medical community is replete with heroes this year, medics who go in harm’s way on a daily basis. What follows here, alas, is not about Covid heroes. This yarn is about the difference between a halo and a noose; the noose of manipulation under the halo of better medical care.
An American physician will either be a DO (doctor of osteopathy) or an MD (medical doctor). By definition, osteopathy emphasizes “the treatment of medical disorders through the manipulation and massage of the bones, joints, and muscles.” The key word here might be “manipulation.” In theory, DOs and MDs are both physicians. In the primary care community, alas, the difference between the halo and the noose appears to a matter of inches not miles.
Without unravelling the historical MD/DO hairball, let’s just say the osteopathy minority has more than a little quackery in their DNA. Think cranial, holistic, wellness, or “hands on” health care.
Concierge medicine now marches under a similar guidon. This boutique, or elitist, variety of health care appeared shortly before the Covid-19 disaster struck. In theory; a Concierge practice, like osteopathy, offers holistic care, a “wellness” component; fewer patients, 24 hour access, same day service, and more “personal” or “quality” time in exchange for an annual fee that is not covered by insurance. The Covid crisis has obviously cancelled many of these alleged Concierge advantages.
Yet, Concierge care is still predicated on up-front, out-of-pocket cash that usually amounts to $2,000 per head per annum.
Call it a cover charge, access, or key money.
If you get referrals from a DO primary to an MD specialist, another boutique aficionado perhaps, you can see how quickly the Concierge model could empty your wallet. The insidious feature of the DO Concierge practice is the ambush. Usually, existing patients are not grandfathered. When a practice goes boutique, the choice is Hobbesian, pay-to-play or take your health care elsewhere.
Access fees are not covered by insurance. Insurance billing and co-pays are separate charges. Concierge fees usually require an auto-pay “contract” too, where billing is automatic, an annual debit.
Absent credit or a handsome bank account, you are definitely not Concierge or osteopath material. Clearly, Concierge practice screens out the elderly, poor, and minorities, if not all disadvantaged demographics. In cities with large ethnic populations, it’s difficult to avoid the discriminatory implications of Concierge medicine.
The convergence of osteopathy, Concierge, and Covid appears to be a merger of revenue streams. Under the “wellness” rubric, DO Concierge practitioners were already marketing various virtual services in the form of remote monitors to be downloaded at home. In the Covid era, such internet applications provide both social distancing and additional revenue opportunities—whilst redefining notions of direct or primary care.
Those “free” wellness apps are replete with webinars, virtual meditation, supplements (with member discounts of course) promotions, and most significantly, data mining with every download. With many Concierge practices, a “video visit,” yet another app download, is required before any office visit. Again, like the pay wall, a mandated video visit is both another virtual barrier and an opportunity to double dip.
With most MD specialists, the video visit is an option, not a requirement.
Statistics on the Concierge or DO hype are hard to come by; data about patient numbers, time spent with patients, or any concrete measures of effectiveness for that matter. “Trust me” seems to be the prevailing ethos. We are assured by wellness flaks, however, that virtual and Concierge medicine is growth businesses.
It’s a good bet that revenue, or an early cash out, not safety or quality care, are the big draws for Concierge practices in general.
Yes, the logic behind those so-called “free” medical apps is revenue and data, not privacy or security. If Bill Gates and Barack Obama can be hacked, most medical apps are about as secure as your lawnmower shed. Indeed, the National Security Agency, just to cite one institutional “metadata predator,” has access to more internet back doors than a colony of beavers.
The Concierge physician is likely to call his service a membership practice where he “treats patients, not disease.” Such bromides raise more questions than they answer. Aren’t all doctors in the wellness business? How do you treat a disease and restrict patients to video visits? If you are ill, wouldn’t you rather be a patient than a “member.” How is medical care better or more personal when pay and virtual walls screen out the most vulnerable or needy clients?
Any physician who is more fearful than his patients midst a medical crisis is clearly in the wrong line of work.
The 2020 pandemic crisis has been especially cruel to the elderly where American medicine has yet to distinguish itself. Liberal politics, not science, seems to be the real spike stimulus behind disgraceful Covid-19 geriatric mortality statistics in New York, New Jersey, and Connecticut.
The likes of Andrew Cuomo and a mute primary care medical community take a bow here.
Politicians like to say that a crisis is a terrible thing to waste. Like state, federal, and public school employees; Covid-19 has provided an excuse for some physicians not to work whilst still getting paid. Withal, we should recall Eric Hoffer, a plebian philosopher, who was candid enough to observe: “Every great cause begins as a movement, becomes a business, and turns into a racket.”
The real danger of manipulative primary care medicine is that any corruption of ethics makes the case for nationalization or socialization of all medical practice.
Additional Reading:
- https://www.beckershospitalreview.com/quality/the-real-problem-with-concierge-medicine.html
- https://www.kevinmd.com/blog/2014/08/direct-primary-care-concierge-medicine-theyre.html
- https://www.youtube.com/watch?v=HRHJnyjm3cw
- https://jaoa.org/article.aspx?articleid=2099490
- https://journalofethics.ama-assn.org/article/ethical-concierge-medicine/2013-07
- https://www.theatlantic.com/health/archive/2014/07/the-case-for-concierge-medicine/374296/?gclid=CjwKCAjwjLD4BRAiEiwAg5NBFg-QSsk_BU6u-8Lqx1gwTiluk6YxyhmKBzUYy_zGFNwdCB8T7ysz4RoCkbgQAvD_BwE
«Previous Article Table of Contents Next Article»
__________________________________
Colonel G. Murphy Donovan (Ret.) is a “member” of a Castle and Connolly Private Health Partners, LLC a medical membership practice in Washington, DC. Formerly, among other Intelligence positions, he was the Chief of the USAF Intelligence Research Division at the National Security Agency at Ft. Meade, Maryland.
Follow NER on Twitter @NERIconoclast